PRACTICE ONE PRESENCE
START HERE . . .
I’m starting with love. I’m starting with breath.
I’m starting with stretching my body that carries me despite the aches.
I’m starting with a hand over my heart. I’m starting with forgiveness.
I’m starting with a clean slate.
I’m starting with a cup of tea and a crisp new page. I’m starting with a tearful release.
I’m starting with wind on my face and gratitude on my lips. I’m starting with my eyes up, not down.
Today, life is calling me to take my own path— Go at my own pace,
Stop when needed,
Notice the signs, people, and sights meant for me. Today, life is calling me to show up—
And I take this brave step by declaring . . .
Love is where I’m starting.
May it also be where I am going. Love IS the way.
Ever since I recovered Google Island, the book I wrote as a child, I’ve been making an intentional effort to connect with that younger version of me, the one I now call “my Dreamer Girl.”
This was the “me” who knew at a very early age that lovingly respond- ing to myself and those around me brought me joy. Over the past few years, I’ve spent time remembering what my Dreamer Girl was like.
She couldn’t walk by a stray cat without talking to it.
She marveled at the sounds she made with her violin and bow.
She loved the rush of the wind when she swung as high as she could go.
She freely ran through the sprinkler in her bathing suit, unhindered by her squarish body that held an abundance of freckles.
And most of all, my Dreamer Girl’s joy was found in filling spiral notebooks with observations, stories, and dreams.
I can’t pinpoint exactly when I decided these inclinations were not acceptable and therefore needed to be abandoned. I’m pretty sure it was during adolescence when I began assuming the roles that gained the world’s approval—roles like the Planner, the Go-Getter, the Accommodator, the Helper, and the Overachiever—and when accolades took precedence over pleasure.
And those roles were just the beginning. In the twenty or so years that followed, I took on so many roles and expectations that it should have come as no surprise when it all became too heavy to bear.
But it did. I can still see myself at my breaking point—the teacher, the partner, the mother, the daughter, the sister, the volunteer, the completist, the juggler, the people-pleaser, the fixer, all simultane- ously coming undone during a morning jog, my well-crafted roles unraveling so quickly I didn’t even try to hold myself together.
Fueling my breakdown was a question I got a lot: “How do you do it all?” I’d always taken it as a compliment, but not on this particular day. At thirty-eight years old, I’d reached the very frayed end of myself, and that question loomed before me, forcing me to stop and face the answer I’d been running from.
I could “do it all” because I missed out on life—I missed out on the laughing, the playing, the creating, the connecting, the memory mak- ing . . . the living . . . the loving . . . and what I missed I cannot get back.
That truth was so gut-wrenching, I was forced to stop. I collapsed to my knees and I wept for all that I’d lost and the desolate place I was in. It was then and there that I decided to tell the truth. Looking back now, I realize the significance of that response. For once, I did not push the pain and discomfort away. I allowed myself to feel it, to let truth enlight- en me, which is why tears of despair turned into tears of relief.
I’d lost my connection with my Dreamer Girl, the tree climber, the notebook filler, the music maker, the seed planter—but she was not gone. Oh no, she was still with me, in here, hand over heart.
I just needed some time . . . space . . . and permission to reconnect with her.
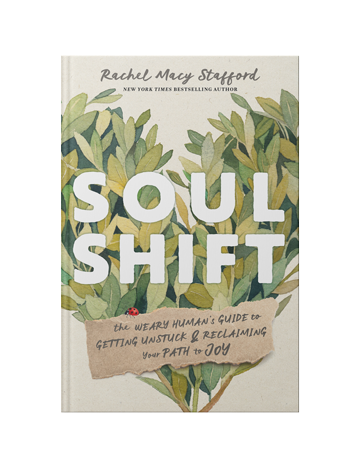
Dear Soul Shift Companion, does that thought resonate with you? Because here’s the reality: as we grow further and further away from childhood, the demands and stress of life increase. We forget we have the power to say yes to what delights our heart and soul, makes us feel alive, and brings us peace. But in order to live an au- thentic, joyful, and purposeful life, we must remember how to say yes to those very things!
We can do it through the Practice of Presence—an intentional choice to temporarily push away distractions and be fully present in the mo- ments of our life.
Within hours of my emotional morning run, I made this choice for myself.
I was in the middle of making lunches. My younger daughter, Avery, who was almost four years old at the time, was on the sofa watching The Lion King. My computer was open, the phone was buzzing, and I was thinking about all the things I needed to do that day. In that moment, I looked up and noticed—really noticed—my child. A clear voice inside me said, “Go be with her. There is nothing more import- ant right now.”
Without closing the bag of bread or looking at the clock, I placed the knife across the jar of peanut butter and went to hold my child.
What happened next was something no one had ever done in my whole life: my daughter brought my hand to her lips and gently kissed the inside of my palm, as if offering a silent but powerful acknowledg- ment of my presence.
This is remarkable, I thought. Tears filled my eyes.
I was so grateful I did not miss that moment and knew I didn’t want to miss any more.
This strong desire to not miss my life is what sparked my Practice of Presence.
Of course, at the time, I did not know it would become my Practice of Presence . . . I called it “going hands free,” a term that was inspired by that kiss-on-the-hand moment.
It might sound contradictory to the process, but being a planner, I needed a plan. Realistically, I knew I could not overhaul my life, give up technology, or abandon all my duties and responsibilities, but that initial response I made to heed the inner voice demonstrated it was possible and practical for me to dedicate small increments of time to just being present.
As an experienced teacher of students with behavioral issues and low self-esteem, I knew the impact of small, achievable steps in creating new, positive pathways. Change begins with a behavioral action, and when you change your behavior, your perspective starts to shift, too.
So, I started with ten-minute periods of time during which I set aside my phone, computer, and agenda to be fully present and open to connection.
It was impossible not to notice how one choice produced a ripple of positive outcomes. For example, after opening my pop-up chair at my older daughter’s swim meet, I chose not to get out my work in an attempt to maximize the free time. Seeing my open lap and available attention, Avery asked if she could sit there. Holding her made me feel at peace and connected to her. When the meet was delayed, I did not fly off the handle because my plan was derailed. Instead, my daughters and I went and asked the coach how we could help, which he seemed to appreciate.
We got home later than expected that night, but I hadn’t yelled or felt that internal pressure . . . which resulted in my falling asleep without the pain of regret. With one choice to be fully present, a series of mean- ingful experiences were created, lasting far beyond a solitary moment.
As I continued to practice choosing connective presence over pro- ductivity, efficiency, distraction, and control, I realized that a feeling of peace consistently came along with that choice; it was as if I was receiving an internal message of encouragement from my soul that said, This feels in line with how I want to live.
Now, does this mean that from this point on life was rainbows and butterflies? Absolutely not. The damaging habits and beliefs I’d car- ried for decades were deeply ingrained, and life continued to deliver unexpected challenges. So, naturally, there were times when I didn’t choose a loving, compassionate, or healthy response to conflicts or big feelings. But . . . I was practicing.
And here was the difference: when I encountered a painful exter- nal clue—a wounded expression, a troubling comment, an upsetting memory, an uneasy feeling—I did not push it away. The difference was . . . I acknowledged it. I allowed myself to feel my response to the discomfort without judgment, so it could be used as information to lead and enlighten me.
Because of this willingness to be present for it all—the remarkable moments and the mundane moments, the peaceful moments and the uncomfortable moments—I was able to move from the painful truth of I am missing my life to a new, healing truth: